Here I am off on my travels again. Not far from my home this time, just a short train ride from Newcastle to Sheffield in Yorkshire. Monika had much further to travel!
Monika and I were invited to attend the DBSNA annual meeting held in the Crowne Plaza Hotel, Sheffield.
We met at the train station in Sheffield and made our way to our hotel where we dropped off our overnight bags and then went to the Crowne Plaza for the meeting which started after lunch.
We were allocated a table where we displayed our mini banner stand and our various leaflets. We were in between Parkinsons UK and Dystonia UK and Tremor UK were also present.
Russell Mills, Deep Brain Stimulation (DBS) nurse and chair of the association opened the meeting by welcoming everyone and thanking them for coming.
Russel Mills DBS Nurse
Sadly we were told that Professor Tipu Aziz who was at the forefront of research into neurological conditions had passed away earlier this year. One of the nurses who worked with him spoke about him with respect and fondness.
We were also told that the association has a new patron, Prof Francesca Morgante, also a friend and advisor for Dystonia Europe.
The presentations then started with a description by a rep from Abbot who told us about the deep brain stimulator they have developed and produced. It uses some new technology and will be available soon.
Next up was someone from Boston Scientific who told us about Image Guided Programming. This utilises images and information that the neuro surgeon has used during the operation, for the nurses to program the stimulator.
After a coffee break we heard from Medtronic who told us about their vision for personalised therapy using Brain Sense for informed contact selection. This helps the nurse to program the stimulator for each patient. Currently they have good data showing how successful this is for Parkinsons’ patients but not much data so far for Dystonia patients.
Professor P Limousin, consultant neurologist at Queens Sq London was next. He told us about the journey of deep brain stimulation and how both the technology and surgery have improved over the years. SubThalamic Nucleus (STN) DBS is still the most popular method but it is not the final solution and more research is needed.
Mr Harith Akram, also a consultant neurosurgeon at Queens Sq London was next up and he spoke about stimulator placement and that technology now allows the STN to be seen on Magnetic Resonance Imaging (MRI) scans aiding the placement of the contacts in the brain. A non metallic frame is fitted to the patients head to improve the quality of the MRI and he is working on speeding up the processing of MRI data such that the patient can be scanned and operated on in the same day.
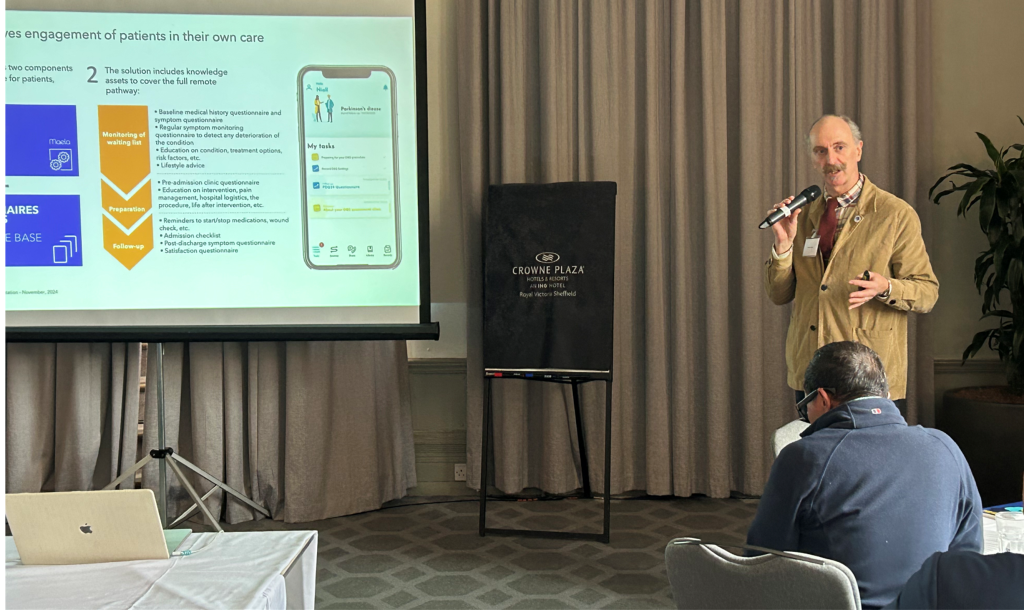
The final presentation for the first day was by Yasmine Yazdani from Machine Medicine who have developed a digital platform for medical professionals to ask patients various questions about their condition, as soon as the patients complete the questionnaire the medical professional can see the reply and act upon any changes required. The patient can also contact the medical professional in the same way.
As this was the last one of the day, Monika and I went back to our hotel to freshen up and change for dinner that evening. We had a lovely three course dinner with wine and a good chance to network with the nurses, consultants and industry representatives who were there.
Day two started with Mr A Hussain consultant neurosurgeon at the Royal Victoria Infirmary in Newcastle spoke about wearable technology for Parkinsons’ patients. This looks a little like a smart watch and measures brain activity by measuring Local Field Potentials (LFP). This can be used before and after treatment to confirm (or not) that the treatment is working for each patient. The patient wears the technology and when they visit their consultant/nurse etc the data is downloaded and analysed.
Next was Mr Jonathon Ellenbogen, consultant neurosurgeon at Alder Hey Children’s hospital in Liverpool. He explained what dystonia is to children and how difficult it is to treat. He does DBS surgery on children but the stimulator is hard to program in children as they can’t always say how they have been, what is better or worse etc. It can take months to get a good
response. Sometimes what is considered a success is simply that the child can now use a tablet. Mr Ellenbogen also used LFP to check the success of the DBS surgery.
He concluded with a video of a child with generalised dystonia before and after DBS, as you can imagine the video was very emotional.
The next speaker was another consultant from the RVI in my home town Newcastle. Miss Claire Nicholson consultant neurosurgeon. I know several dystonia patients who Miss Nicholson has operated on and they all sing her praises! She spoke very well about her main interest of DBS in Dystonia and explained that no 2 patients are the same and therefore there must be an individual approach to programming the stimulator. She explained that the average frequency used is 130 Hz but the pulse width of the signal is not defined. The amplitude of the signal is altered when programming the stimulator but the pulse width could also be altered, however no-one really knows which is best. If the pulse width is widened then lower current is required and vice versa. Miss Nicholson always aims for the lowest signal amplitude which gives the best results. I am a bit biased as I already knew of Miss Nicholsons work but she did give a really good presentation and she really knows dystonia and her patients.
After a coffee break we heard from Tom Payne, a clinical lecturer in neurology based in Sheffield Royal Hallamshire hospital. He spoke about Parkinsons in young people and took us through a case study of a young woman who had symptoms at 23 or 24. Her symptoms were quite mild at first but soon progressed to the point where she could no longer work. She also developed severe left sided dystonia. Her parkinson’s symptoms responded well to Levodopa but her dystonia worsened. At age 30 she had DBS which was successful but then a few years later her symptoms returned and worsened. She now uses a wheelchair to get around and despite her symptoms is enjoying life and recently got married.
Claire Nicholson consultant neurosurgeon
Caroline Robbins a nurse specialist from North Bristol NHS Trust spoke next. Caroline explained how remote programming works really well. She connected with a patient and we could all see her on the screen. Caroline and her were able to talk and Caroline could give advice, I’m sorry but I am not sure if the clinician can also alter the stimulator remotely or if they advise the patient how to alter their stimulator themselves. I think by this time my brain had reached saturation! However I am sure of the advantages of remote connections between patient and clinician, there is no travelling involved for the patient, especially good for those who live a long way from a treatment centre, it also reduces clinician time compared with an appointment in a clinic.
After lunch we heard from Russell Mills again, as well as being the Chair of the Nurses Association he is also a nurse specialist in DBS in the RVI Newcastle. Russel spoke about the Get-Ready remote patient management by Medtronic. Russell is currently managing several patients using this system, similar to other remote patient access programmes, the patient and the clinician can send each other questions and answers. This system also reminds patients what they need to bring with them when they come to hospital for their DBS surgery and what to expect after surgery.
Mr B Miraz was next and he is a consultant neurosurgeon in the Royal Hallamshire Hospital Sheffield. He took us through a case study of a female in her 30s who has hemi-dystonia. The pain and twisting in her foot was so bad she considered amputation in 2018. She had DBS instead and had enough relief from that she didn’t need to think about the drastic step of amputation!
Kelly Storey is a Parkinson’s specialist nurse and spoke about the use of Pro Duodopa to treat Parkinsons’ patients. This is a new drug available on the NHS (National Health Service in UK) which is showing good results but there are some side effects. The drug is very expensive, costs around £60 000 per patient per year so as you can imagine there are strict criteria that any patient has to meet before being prescribed Pro Duodopa. It has caused a skin reaction in some patients and 2 of the 8 patients she has prescribed Pro Duodopa for have stopped taking the drug. Clearly even at that price it doesn’t suit every patient.
Monika and I had to leave at this point to get our transport home, my train to Newcastle and Monika’s train to London where she was staying for a few days well earned break.
The conference was a huge success, well attended, great speakers and presentations and of course lovely meals and snacks. For Dystonia Europe it was successful in that lots of people came to talk to us and took leaflets away with them and we connected with at least 2 consultants who agreed we can stay in touch, hopefully they will agree to do a webinar for us soon. Personally the highlight for me was understanding the technology! My background is in engineering although I haven’t worked in engineering since dystonia started for me in my mid to late 40s, it was very reassuring for me when I realised I understood most of the technical side of the stimulators. Another highlight for me was using the simulator made by Boston Scientific and Brainsense, I put on the special headset and was instantly transported to inside someone’s brain! I could walk through it and look around, it was amazing!
I wonder what the technology will be like the next time we attend this conference in 2025?

Gill Ainsley, Vice President and Secretary, Dystonia Europe
