Enrico Saibene, A. Crippa, M. Ramella, G. Giacobbi, C. Corrini, D. Anastasi, A Castagna
Isolated Cervical dystonia (ICD) is a movement disorder characterised by intermittent or sustained involuntary contractions that cause altered postures or abnormal movements, also tremors, of the head, neck, with occasional involvement of the shoulders. For about thirty years, the efficacy of botulinum toxin as symptomatic treatment of this pathology has been demonstrated, but there are still no shared guidelines regarding the role of rehabilitative interventions. Although the combination of different rehabilitation techniques such as passive mobilisation, muscle stretching, antagonist muscle recruitment, relaxation techniques, and the use of biofeedback for motor control are suggested as useful in dystonia in several studies, there are no clear guidelines about definition of goals of treatment and outcome measures due to the lack of standardised protocol studies.
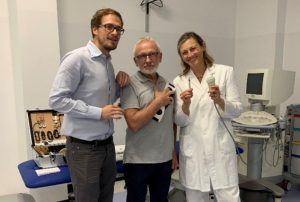
From 2014 in the Research Hospital Fondazione Don Gnocchi Santa Maria Nascente of Milan, in Italy, thanks to the strong collaboration between a neurologist expert in cervical dystonia, motor learning strategies and botulinum toxin treatment, Dr Anna Castagna, a PMR doctor Dr Marina Ramella with a special expertise in visuo spatial and perceptive rehabilitation and a group of talented physiotherapists, Alessandro Crippa, inventor of biofeedback system Leonardo, Giulia Giacobbi, Chiara Corrini, Denise Anastasi and Enrico Saibene expert in perceptive approaches, an effort in the field of rehabilitation treatment of ICD has been conducted firstly with a pilot research protocol, and then with a transfer over the years into the daily life clinical practice, treating hundreds of persons with iCD successfully.
The goal of the first study published on Clinical trial.gov NCT03247868 was to evaluate the effectiveness in the same patient of a combined sensorimotor relearning strategy using biofeedback techniques and visuo-spatial rehabilitation, (SPRInt, Sensorimotor Perceptive Rehabilitative Integrated program) in conjunction with BoNTA injection versus the gold standard botulinum toxin treatment. This pilot study, published as an original paper in 2019 in Neurological Sciences verified that SPRINT and BoNTA gave iCD patients a significant increase in the quality of life compared to therapy with botulinum toxin alone, in terms of quantity and duration of benefit.
In detail this trial was designed as 6 months duration and was conducted, involving 11 patients (5 males and 6 females) with isolated idiopathic cervical dystonia. Each patient initially undergoes a neurological evaluation and is injected with botulinum toxin according to a personalised scheme (T0), then re-evaluated at 6 and 12 weeks (T1 and T2). At time T2, each patient is again injected with BoNT and begins a rehabilitation cycle according to the SPRInt rehabilitative approach (18 sessions, three times a week, lasting 45 minutes each). At the end of the rehabilitation cycle (T3) and as a follow-up (T4), 6 months from T0, each patient is re-evaluated. Each clinical evaluation is associated with cervical district kinematic analysis and the administration of three scales: Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS severity, disability, pain), EQ-5D5L for quality of life, and Self Anxiety Scale (SAS), to assess patients’ psychological characteristics.
Results
Preliminary data obtained in the pilot study show that at the end of the evaluation period (follow-up), the painful symptoms, the severity of the pathology, and the disability resulting from the disease are reduced compared to the initial evaluation. In particular, the total score of the TWSTRS scale, from 39.0 ± 10.9 (calculated data with median and IQR) at T0, decreased to 30.50 ± 17.75 at follow-up (p<0.01). Performing post-hoc analysis of the data obtained for each field evaluated within the TWSTRS, it was observed that the disability reported by the patient decreased more after combined treatment (SPRInt), compared to treatment with botulinum toxin alone, and that this change was partially but significantly maintained at follow-up (p<0.01). The severity of the pathology was reduced after combined treatment, from a score of 19.0 ± 4.5 to 12.0 ± 5.0, partially persisting over time (14.0 ± 3.5), while regarding the painful symptoms, there was no variation after combined therapy compared to sole botulinum toxin injection.
Conclusions
Although botulinum toxin currently represents the gold standard in the treatment of isolated cervical dystonia, the effect of the drug is not long-lasting and totally effective for the complete resolution of the complex symptomatology complained of by the patients which presents different motor and non motor phenomenology. The experimental SPRInt approach inspired by the concept of sensorimotor relearning through feedback and visuo-spatial rehabilitation focused on personalised goals and specific needs, could interact more effectively with dystonia complexity, improving the quality of life of patients. Regarding painful symptoms, botulinum toxin seems to represent the most effective solution. Furthermore, further systematic research is needed to clarify the role of rehabilitation within the treatment of dystonia and to give the people affected the opportunity to be treated all over the world with tested and specific exercises in conjunction with botulinum toxin injections.