A variety of treatments are available for people living with dystonia; deep brain stimulation (DBS) can be a beneficial treatment option for improving their quality of life. The treatment involves the placement of two electrodes into the brain, connected by a wire under the skin to a stimulator, usually placed in the patient’s chest or abdomen.1 The DBS system delivers targeted electrical impulses to specific regions of the brain, to block signals, resulting in improvement of dystonia symptoms.2
Guide-XT, a new visualisation software developed by Boston Scientific, is being utilised by a team at the Würzburg University Hospital in order to optimise DBS programming and significantly reducing the time required to deliver the best results for patients. We discussed their work using visualisation software, such as Guide-XT, with Professor Jens Volkmann, Full Professor and Chairman; Dr Philip Capetian, Senior Consultant, Head of DBS Outpatient Clinic; and Dr Martin Reich, Junior Research Group Leader. Prof Volkmann believes: “DBS is the only therapy that is targeting the cause of dystonia,” supported by Dr Reich who emphasises that: “Visualisation software will change the way we programme patients in the future.”
Visualisation software is the Google Maps for DBS
To understand how visualisation software, such as Guide-XT, works, Prof Volkmann explains: “The impact of DBS is all about location. You need to know exactly which few cubic millimetres of tissue in a certain area need to be stimulated to produce the best possible effects and to avoid adverse effects. In a way, it [visualisation software] is like GPS or Google Maps: it helps us to orient ourselves in 3D space.”
The benefits of this are multifaceted, including confidence in placement to avoid adverse effects and to achieve optimal results: “Having an anatomical programming approach at our fingertips is really making things easier. It has already changed our approach, especially for dystonia patients… we gained a lot of confidence to programme,” explains Dr Capetian.
Time can be a significant barrier when programming DBS, but with Guide-XT, this issue is irradicated, as Dr Capetian adds: “In the past, I needed to test the patients, and for dystonia it was a bit problematic because you wouldn’t have immediate responses… now you really know where your electrodes are located, and you can simulate the field you can achieve with stimulation.” Therefore, physicians can achieve optimal results from your initial visit.
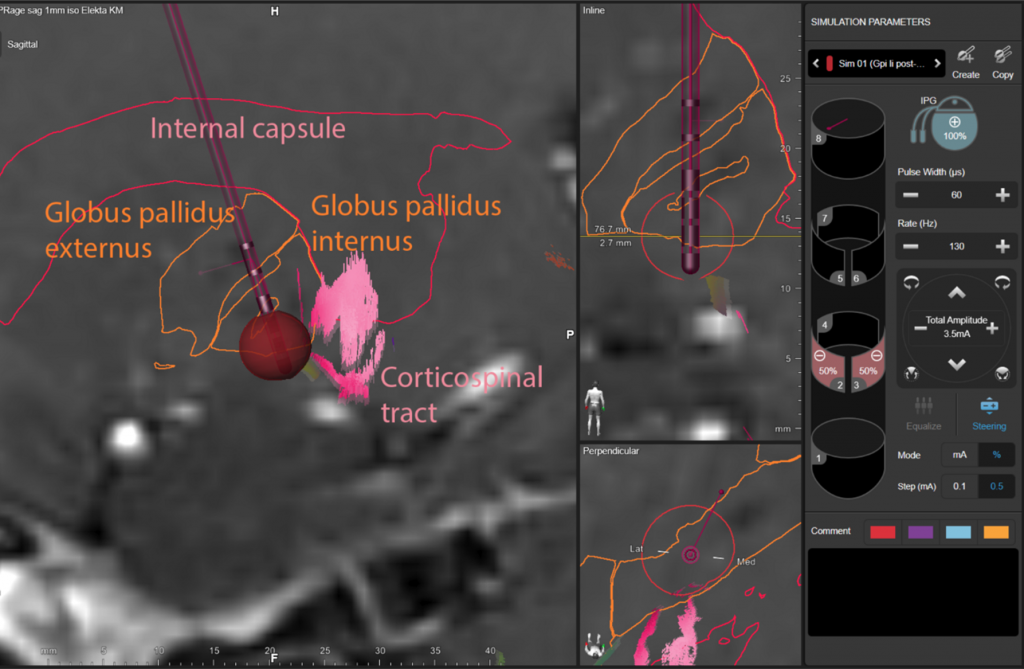
Overview on the left Globus pallidus internus (GPI, orange) with stimulation electrode (red) in place. Surrounding structures, segmented for this patient’s specific anatomy. The programming settings created by the physician are displayed on the right side of the screen and represented in red on the image on the left as the region that will be activated to provide the best outcomes for the patient.
Tapping into Big Data
Guide-XT has an impact that goes beyond individual patient cases. “We are in an era of digital revolution and we should learn from the approaches that come from totally different fields,” says Prof Volkmann. We are starting to see the impact of Big Data in other industries, and the potential in healthcare is seemingly infinite. With the Guide-XT system, we can pool data to improve diagnosis and treatment pathways.
This pool of data is already being captured and having a positive impact. Dr Capetian explains: “For many years, we have been collecting outcome data from our patients, so we have been collecting pre-operative data from all of our DBS patients and we have been collecting the clinical outcome data in a very broad sense and now we are starting to analyse the imaging data.” By harnessing the data of many patients, physicians can see the bigger picture and use this to more accurately treat a wider range of patients: “This can inform programming because you can create maps of multiple patients where you see certain responses or adverse effects,” adds Prof Volkmann.
What are the benefits of this personalised treatment for people living with dystonia?
Prof Volkmann believes that patients are put off because “they are afraid of adverse effects.” These adverse side effects are caused if the electrodes are not positioned in the optimal area of the brain or if they are inappropriately programmed – both of which are difficult to predict; however, visualisation software has changed the game for patients. “We can look at the images and verify the lead position and then make an educated choice. That is the big difference. This educated choice is much more likely to get a good clinical solution, in a much shorter time,” says Prof Volkmann.
This software is not just benefiting newly diagnosed dystonia patients, but also those who have established good outcomes, as Dr Reich recalls: “I remember a dystonia patient who had a really great response to DBS; she had 80% of symptom control, but at this time she had a little bit of cervical dystonia, which she suffered from and had a lot of neck pain. We went to the visualisation software and saw that the DBS electrode was nicely placed but we were stimulating too deep, so we changed it. This was a game-changer, for me, it wasn’t a troubleshooting case, but it was an efficacy case where she was already a good responder.”
Like most things within healthcare, this is not a ‘one size fits all’ treatment, and Dr Capetian reminds us that Guide-XT with DBS can provide targeted, individualised medicine: “We cannot make everything perfect by using our approaches and anatomy-based programmes, but most patients have some benefit…even patients out there who have been unhappy for years and years.”


